Hello, i am female 27 years old. after a months of terrible bone pain and muscle spasms i was diagnosed with celiac disease. But 3 weeks after diagnose, my control blood work showed low leukocytes (3,6). One month before it was 5.1! Is there something to worry about? I am really concerned since i have terrible bone pain, i am on gluten free diet only 14 days. I know that bone pain is quite common for silent celiac disease but i am worried it might be cancer also. My alkaline phosfate was in normal range (0,89). My calcium was month ago low (2,07) and now is normal (2,42) but such increasing is worrying me it might be osteosarcoma or multiple myeloma. I have to say that my bones hurts all over the body. Sometimes fingers (hands) sometimes long leg bones. I am low on D vitamin, my B12 wasnt checked. Thank you so much!!!
Oncology
Stage 2 throat and neck cancer, undergoing chemo and radiotherapy, need second opinion?
My partner is a 59 year old male who was diagnosed with stage 2 throat and neck cancers three months ago.
The tumors we can see are obviously around his throat but go around his ear and the back of his head.
We know he has tumors on his sinus and tonsils.
He has lost the ability to swallow and his speech is all but gone, he has a constant headache that prevents sleep, he is in agony around his face and neck/shoulders.
So far he has done one session of chemotherapy and four radiotherapy however, it hasn’t decreased his tumors as they are now three times the size!!!
Before he started treatment he experienced momentary blindness and halucinations.
Initially the doctors gave him oxycodeine but then declined to give him more as they said his throat is going to close and they plan to keep him in hospital on a morphine drip!!!
Now I am worried that they are putting him through chemo and radiotherapy for naught.
Is it possible that the cancer is spreading and can it spread to the brain?
Diagnosed with a heart fibro-elastoma , 50-50 chances it is cancer, how to take this thing forward?
My mother was diagnosed with a fibro-elastoma (1.5cmx 2cm) in PML of heart about an year ago. It was an accidental discovery during the clearance for surgical removal of a lipoma in left underarm. She had no symptoms except for prolonged mild fever which has stopped since the last 3 months. Recently a growth in the tumor (about 0.5cm) was reported through echo. The doctor advised Cardiac MRI.
The Cardiac MRI gave a different picture.
The size is about 2.5 to 3 cm (about 0.5cm growth in an year)
The tumor is not attached to any valve, instead it’s on the inner side of heart chamber (no damage to the heart wall)
The radiologist says its giving a very high contrast which means its vascular
They say it could be connected to the lipoma in her underarm(the lipoma was diagnosed through biopsy an year ago)
They say there is a 50-50 chance that the heart tumor is cancerous, and to confirm a biopsy will be done of the tumor which requires open heart surgery
We need your advise on how to take this thing forward. The tumor has been there for about 1.5 hear without a growth like that of cancer and my mother is normal without any symptoms except for Diabetes, high blood pressure and plus she is over weight .
Your help in this regard will be highly appreciated
After lumpectomy, lymph node surgery and radiation therapy, I have stabbing pain in lower back?
I am a 49 year old female. Last December I was diagnosed Stage II Breast cancer, they found a micro- metastases in my lymph node on the affected side. I had lumpectomy and lymph node surgery in January, followed by 8 weeks of radiation, no chemotherapy. Since about April I have been experiencing a stabbing pain in my lower back, the exact same spot each time. It only lasts a few seconds and dissipates. But it recurs often, several times a day. This morning alone is has been occurring several times per hour. My medical oncologist thinks it must be muscular. is it possible to experience nerve damage in my back from lymph node surgery?
My father has hairy cell leukemia blood clots formed in belly, how to stop pain and clots?
My father is 53 years old, a month ago he saw some swelling and after two days he saw blood clots in his leg. he went to doctor, they said he diagnosed with superior venues thrombosis. then after further blood testing they fund out he has hairy cell leukemia. right now he is taking wafarin and enoxaprin sodium injection, but in his belly there is blood clots formed what he can do to stop the pain and clots? help us please.
I had ovarian cancer and reflux surgery I still deal with constant nausea. I can barely eat, and I am unable to live life and go anywhere?
In 2009, I had surgery to remove a very large ovarian tumor (it was a rare cancer that grew big but did not spread, so I was left with one ovary). They made a vertical cut down my entire midline from just under the breastbone all the way down past the belly button. After I recovered, I felt fine, although my abdominal muscles stuck out some, of course. In 2010, I got pregnant and had constant nausea throughout (which at the time I attributed to the pregnancy). I had a C-section in 2011. After the C-section, I still had the constant, debilitating nausea and couldn’t function. It never went away. I had an upper endoscopy done, which showed evidence of GERD (I had wearing away of the esophagus). I tried all sorts of over-the-counter and prescription meds for reflux and nausea, but none helped. A couple years later, I had a laparoscopic Nissen surgery done (which wraps the stomach around the LES to prevent reflux). The surgeon said I had a small hernia, which he did not fix since he said it was very small. I had slight improvement after my reflux surgery, but not much. I still deal with constant nausea. I can barely eat, and I am unable to live life and go anywhere. I am housebound, and at times, bedridden. I am only 38 years old. Obviously my abdominal muscles were cut in half vertically during the tumor surgery of 2009. I suspect that the pregnancy made things worse. I still have some protrusion of my abdominal muscles, as my belly sticks out, as though I am pregnant (I’m not). I’ve tried to do rehab exercises for a possible diastasis recti, but this only causes more nausea. Is it possible that a small hernia and/or diastasis recti could cause this constant nausea? Is there anything else, anatomically, that could be out-of-whack? Could the stomach be pushed out and thus not be in the right position? Is there anything that can be done to fix my constant nausea? It’s not something I can live with. (My ovarian cancer is not the cause, since I’ve been tested, and it has not come back.) Please help!
MRI showed a 9 mm lesion in my head inadvertently?
I am female aged 54 but still quite fit after having problems with my ears after a severe ear infection I was sent for a hearing test and an MRI to be on the safe side . This came back normal but they inadvertently found a 9 mm lesion in my head I’m unsure of where abouts as I didn’t understand the terms used but was told it shouldn’t be where it was . My consultant then said if it were his relative he would want an advanced MRI with dye injected . This seems rather a large lesion and I’m worried I have been getting stiff neck regularly also and wandered if it’s a symptom thanks for any help.
My father has been diagnosed with brain tumor – requires surgery, medication or other treatment?
Age-62 Yrs
Gender-Male
Diagnosis-Brain Tumor
Question: My father have been diagnosed with brain tumor. Moreover, he has also a diabetes. How diabetes effects during treatment of brain tumor? I heard above 60 year of age, its very difficult to do surgery, is there any other treatment or medication to kill the tumor cell? While report says Tumor cell is not within the brain. Please advice me.
I had a small swelling in the right breast, Is this lymphadenopathy significant
I m a 22 year old female I had a small swelling in the right breast 14*9mm .. with non specific axillary lymph node 22*8 mm on rt and 20*5 on the left. Is this lymphadenopathy significant.. but from d impression of us it says it’s a fibroadenoma of BIRADS 3? I want to know if the lymphadenopathy is significant and if is so.. whats the probable reason for it being on b.s
Lost 30 pounds without trying. I’m extremely tired all the time. Nausea and vomiting?
35 year old male. I’ve had a headache for the last 4 months. Lost 30 pounds without trying. I’m extremely tired all the time. Nausea and vomiting. I have Hashimotos Thyroiditis. Total thyroidectomy 3 years ago. My PCP isn’t really helping. I’m wondering what could be causing my symptoms?

Had chest CT scan , primary care provider thinks it is fluid or an infection, can it be cancer?
I received the following report from a chest CT scan: There is evidence of a 3.2 cm x 1.6 cm x 2.5 cm irregular infiltration in the peripheral aspect of the superior segment of the left lower lobe. Air bronchograms are seen within this. This may represent a focal pulmonary infiltrate. Underlying mass lesion can not be ruled out. There is no demonstrated pleural abnormality.
What does this mean? The nurse said the my (primary care provider) PCP thinks it is fluid or an infection and not likely to be malignant. I am still worried. This seems very large and I don’t have symptoms of pneumonia. How concerned should I be that this is cancer? I am a 40 yo, female with no smoking history. This was initially found on a routine work x-ray. How should I proceed?

I had radiation therapy and chemotherapy for stage 4b2 cervical cancer, Is it possible my ovaries weren’t completely fried and I’m ovulating again?
I’m 34 years old and was treated with radiation and chemo 2 years ago for stage 4b2 cervical and haven’t had a menstrual cycle since as expected. Went through all the changes my gyn/onc explained. Then a week ago I began bleeding again. I just last month a a clean exam and pet scan. Is it possible my ovaries weren’t completely fried and I’m ovulating again?

I have an enlargement of prostrate, can Calutide be prescribed for BPH (Enlarged Prostate)?
I am a male ageing 57 years old have been suffering from enlargement of prostrate for last 2 years. During October 2015 my PSA was detected at 10.92.Thereafter I underwent TRUS and prostrate BX. But it revealed no sign of malignancy. However immediately after Prostrate BX , I was fallen acutely sick with complete retention of Urine. Accordingly, I was hospitalized in January 2016 and treated with iv injection and catheterization. At the time of discharge after one week with catheter in situ, I was advised to go for TURP at the earliest. However, I was not in favor of surgery. Hence, I had made consultation with another surgeon in last week of January 2016 and based on his advice I have undergone MRI Prostrate .PI Rads of MRI is 3/5. Depending on the report, he prescribed me the medicine CONTIFLOW-D and advised me to report after 1.5 months with PSA Report. Accordingly, I made report to him in FEBRUARY 2016 WTH MY PSA reading at 8.05. On going through the report, the doctor removed my catheter, prescribed the same medicine –CONTIFLOW-D, and asked me to report again in May 2015 with PSA REPORT. On 7th.May 2016, I visited the doctor with PSA reading at 6.05.The doctor then prescribed me Urimax-D and Calutide-50. in replacement of the earlier prescribed medicine. However on consuming Calutide-50, I being a bronchial Asthma patient, developed breathing problem. Accordingly, I made my PSA test on 13.06.2016 and visited doctor on 15.06.2016 with PSA report of 2.72 .On going through the report the doctor advised me to continue other medicine excepting Calutide and report after 03 months with report on PSA and Haemoglobin. I have made my PSA and haemoglobin on 02.11.2016 and the report of test reveals that PSA has been elevated to 5.27 while haemoglobin % has also increased from 14.0 to 14.4.With the report I have consulted my Urologist on 05.11.2016 and due to elevation of PSA he has advised me to continue Calutide again.
I have learnt from my chemist that the medicine Calutide is generally prescribed for treatment of Prostate cancer. I am rather worried if I have been suffering from the said Incurable disease.
In view of the above, kindly inform me if Calutide can also be prescribed for BPH.
Regards

Suspected to have a lung cancer fine needle biopsy found a few atypical cells and no malignant cells?
I am sending this question for my mother in law who has been suffering from cough for about 2 months. She was suspected to have a lung cancer since the CT scan reveals several nodules on her lungs. She was tested for sputum and came out negative. She also underwent fine needle biopsy but it did not rule our the carcinoma even though they only found a few atypical cells and no malignant cells are found. What other tests can we do to confirm or totally rule out the possibility of having a cancer? Aside from lung cancer, what are the other possible illness that has these same symptoms? Does the attached biopsy insufficient to rule our carcinoma? She is 57 years old.


My mother is diagnosed with (G2) adenocarcinoma stomach, is chemotherapy the best option?
Hi. My mother is 44 and has been recently diagnosed with (G2) adenocarcinoma stomach. There is no visible bleeding. Just internal bleeding through stool.
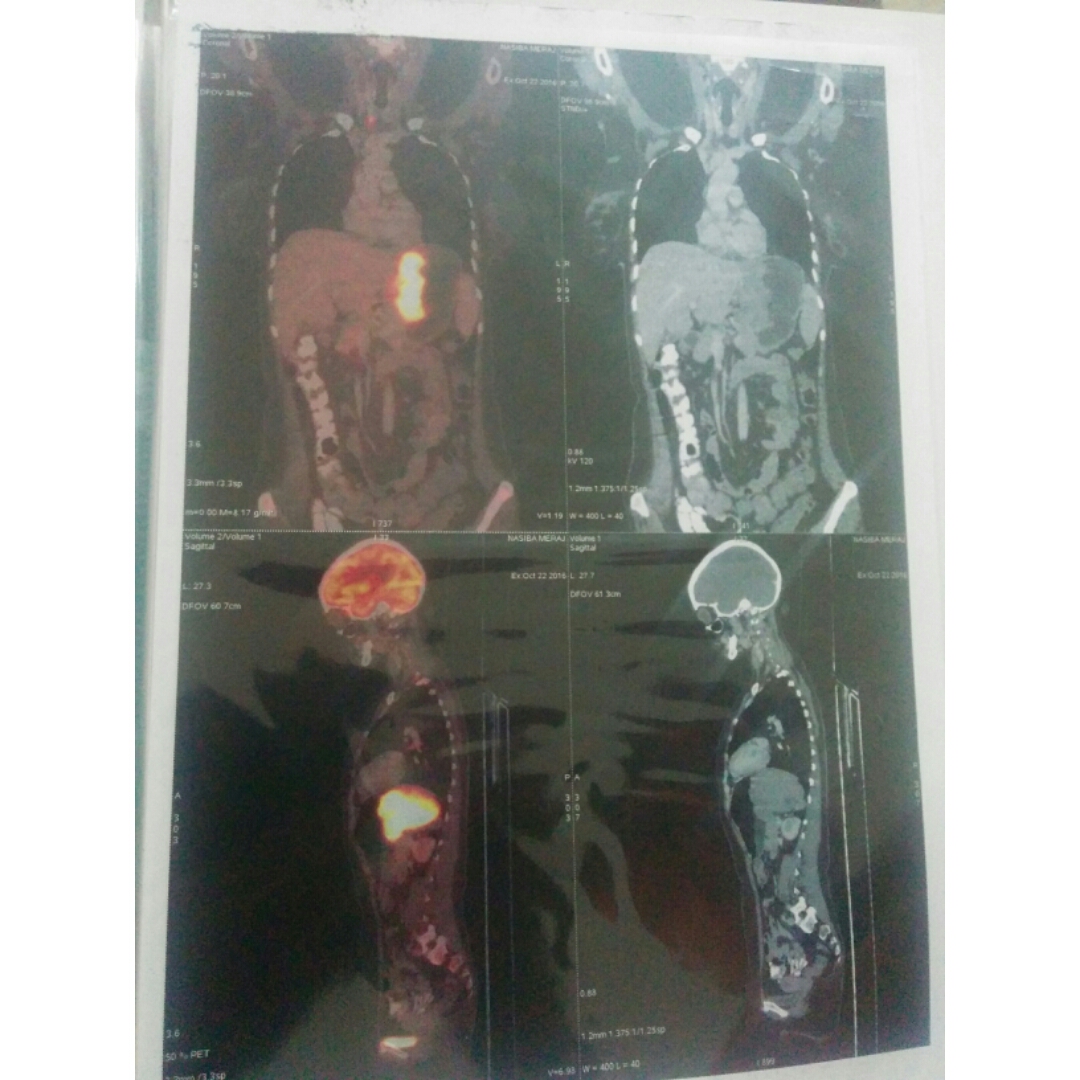
I’m posting her PET scan review:
bove scan was reviewed and the following comments were offered.
Finding:
Stomach shows irregular wall thickening involving cardia, fundus & body along lesser curvature of stomach
(thickness 4.0 cm, SUV max 14.6). It is abutting the inferior surface of spleen. Fat planes between stomach
and spleen appears lost at places.
Few mildly metabolically active perigastric lymphnodes are seen (largest 1.6 x 0.7 cm, SUV max 4.3).
Increased tracer uptake was seen in level VI lymphnode. This appears unrelated to primary disease process.
Right lung upper lobe shows a calcified nodule. Rest of the both lungs are unremarkable. No metabolically
inactive or metabolically active nodules or infiltrates are seen.
Trachea and main stem bronchi appear unremarkable. There is no evidence of pleural effusion or metabolically
active pleural abnormalities.
A subcm metabolically active superior mediastinal lymphnode is also seen (SUV max 5.2).
No metabolically active lesions were seen in nasopharynx, oral cavity, oropharynx, larynx and hypopharynx.
Major salivary glands appear unremarkable. No metabolically active lesion was seen in the thyroid.
No significant metabolically active cervical lymphadenopathy was seen.
Liver shows physiological tracer distribution. No significant metabolically active lesions were noted in
both lobes of liver.
Gall bladder is visualized. No significant metabolically active abnormalities are seen in gall bladder.
Spleen shows physiological tracer distribution. No metabolically active lesions were noted.
No metabolically active abnormality was seen in the pancreas.
Bilateral adrenals and kidneys are unremarkable and show physiological tracer distribution.
Small and large bowel shows physiological tracer distribution.
No metabolically active abnormalities were seen in the mesentery.
REVIEW OF OUTSIDE PET-CT
Rectum shows physiological tracer distribution.
No significant metabolically active pelvic lymphadenopathy was noted.
Both axial and appendicular skeletal system show physiological tracer distribution.
Urinary bladder is not well distended and show physiological tracer distribution.
Rest of the body shows normal physiological tracer uptake.
IMPRESSION:
1. Metabolically active stomach wall thickening (with extension & involvements) with perigastric lymphnodal
involvement as described.
2. No other metabolically active disease elsewhere in the body.
Her haemoglobin count is 6.6 due to which doctors suggested to go for chemotherapy.
I wanted to know if it’s the best option? What would be the success rate of the treatment. Is there any other alternative?
Thank you.